論文のあらすじ
口の中が燃えるように痛い症候群は、粘膜に異常があることや口腔乾燥、味覚障害を伴うこともありますが、全身的な慢性の病気やストレスなど心因的な要因も大きく影響します。
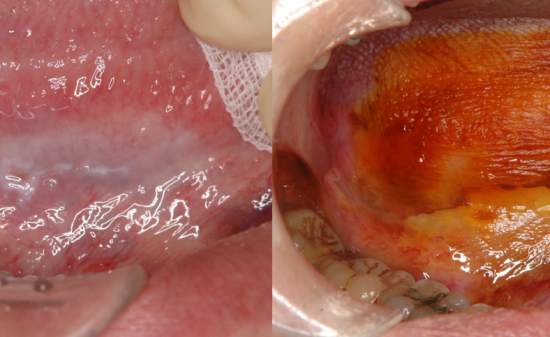
口腔灼熱症候群(BMS;Burning mouth syndrome)は口腔内が燃えているような、または刺すような感覚が特徴の疾患であり、舌、口蓋前方部、口唇に症状が出やすいとされている。以下の論文では口腔乾燥症や味覚障害とも関連があり、BMSを有する患者さんはBMSを有さない患者さんと比較して体調の不良、強迫観念、うつ症状、不安、ストレスを訴える方が多く、また慢性疾患を有している割合が優位に高いことを示した論文である。結論として心理的要因とBMSとの関連性が高いことを示している(Dr. 曽我)。
論文内容
Int J Oral Maxillofac Surg. 2018 Mar;47(3):374-378. doi: 10.1016/j.ijom.2017.09.012. Epub 2017 Oct 23.
The role of psychological factors in the development of burning mouth syndrome. Yoo HS1, Jin SH2, Lee YJ1, Song CM1, Ji YB1, Tae K3.
The psychiatric profiles of 50 patients diagnosed with burning mouth syndrome (BMS) were compared to those of 50 age- and sex-matched individuals as the control group. The Symptom Checklist-90-Revised (SCL-90-R) questionnaire was used to evaluate the role of psychological factors in the development of BMS. Somatization, obsessive-compulsive, depression, anxiety, hostility, phobic anxiety, psychoticism, global severity index (GSI), positive symptom total (PST), and positive symptom distress index (PSDI) scores were significantly higher in the patients with BMS than in the control group. In a subgroup analysis according to sex, women with BMS had higher T-scores for somatization, obsessive-compulsive, paranoid ideation, GSI, PST, and PSDI than women in the control group. In contrast, only the PSDI score was significantly higher in men with BMS compared to men in the control group. There was a significant difference in the T-scores for somatization, psychoticism, and GSI between the three age subgroups (≤50, 51-65, and ≥66 years). The obsessive-compulsive and PSDI scores were significantly higher in patients with BMS who also had at least one chronic disease than in patients with BMS who had no chronic disease. In conclusion, psychological factors are correlated with BMS.



















 PAGE TOP
PAGE TOP